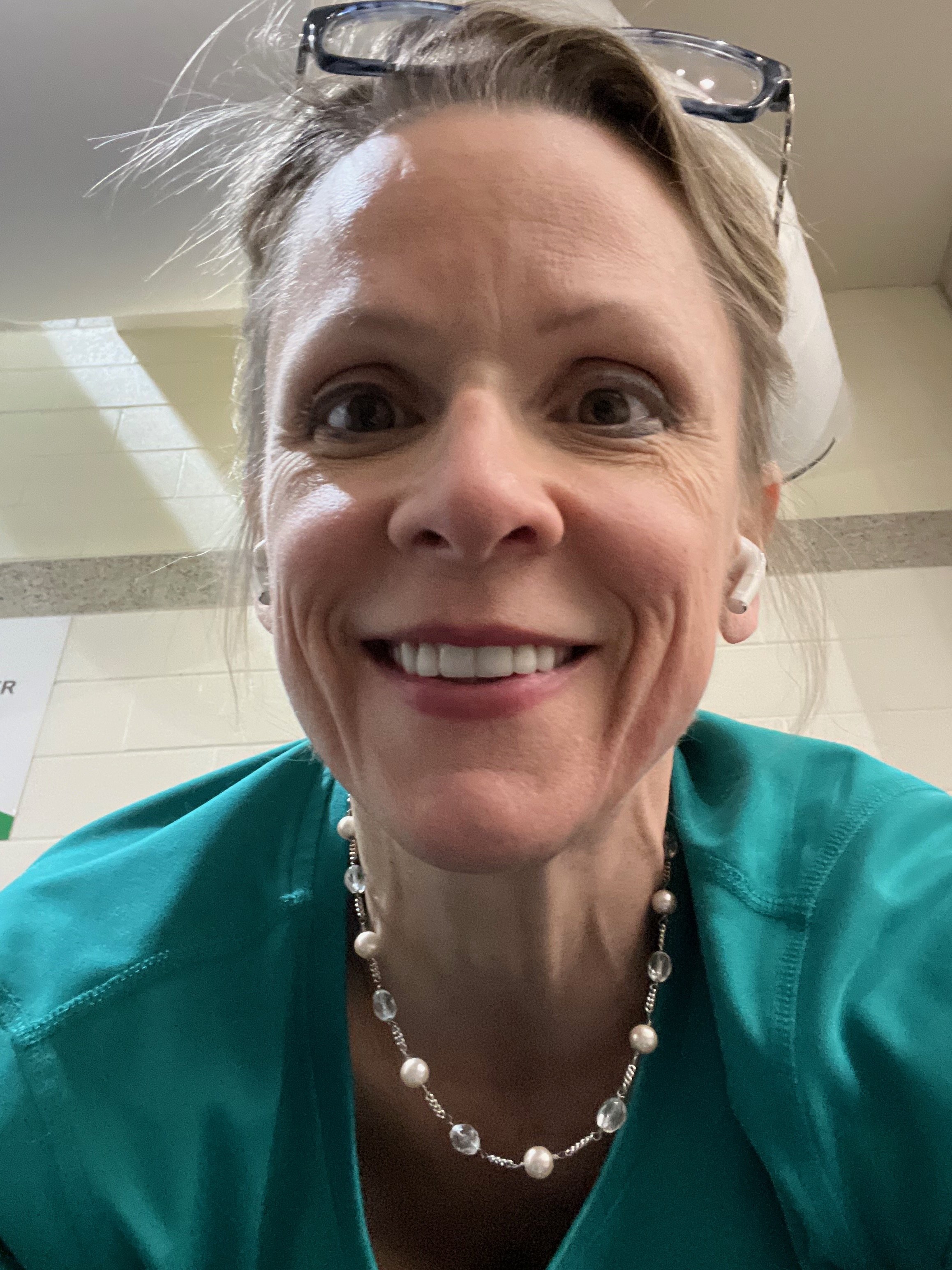
Bridget, Certified RN Anesthetist and Gadolinium Researcher
Bridget, a certified registered nurse anesthetist with a background in chemistry, was diagnosed with fibrotic nodules following multiple MRI macrocyclic gadolinium doses for cancer monitoring. Her case demonstrates that gadolinium-induced fibrosis is possible even with newer contrast agents and normal renal function. Faced with a lack of medical support and research regarding gadolinium toxicity, Bridget took it upon herself to research gadolinium and seek life-saving treatment. After all the research that Bridget has done for this website, she realizes that the scope of this iatrogenic condition is broader than she could have ever imagined.
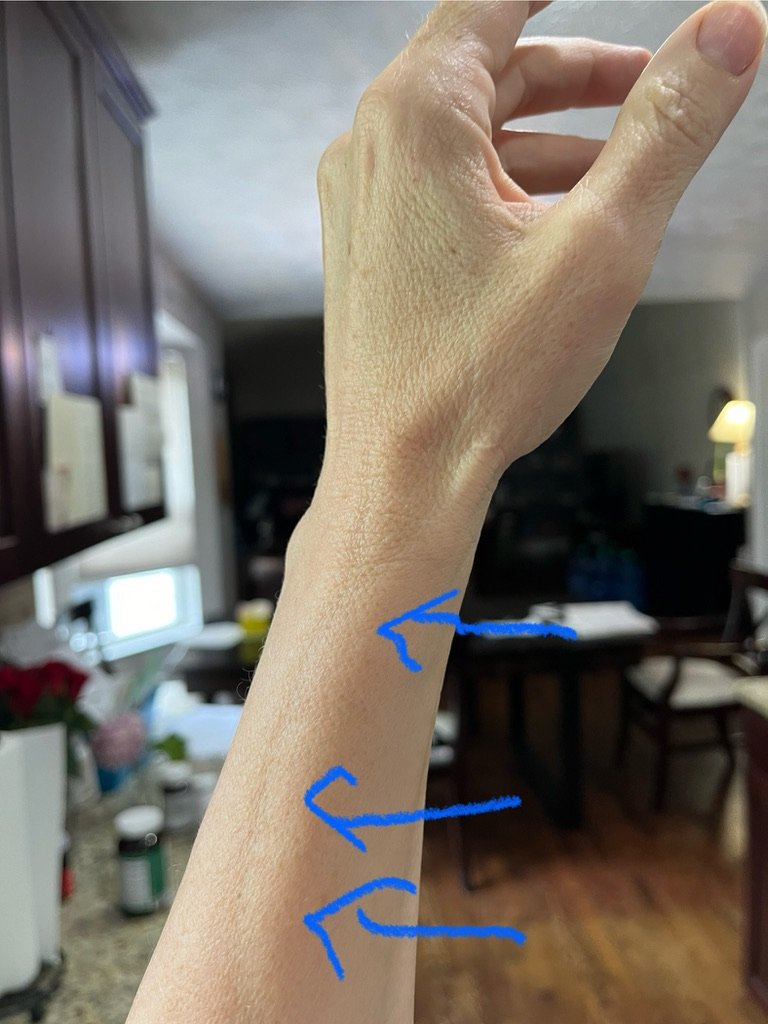
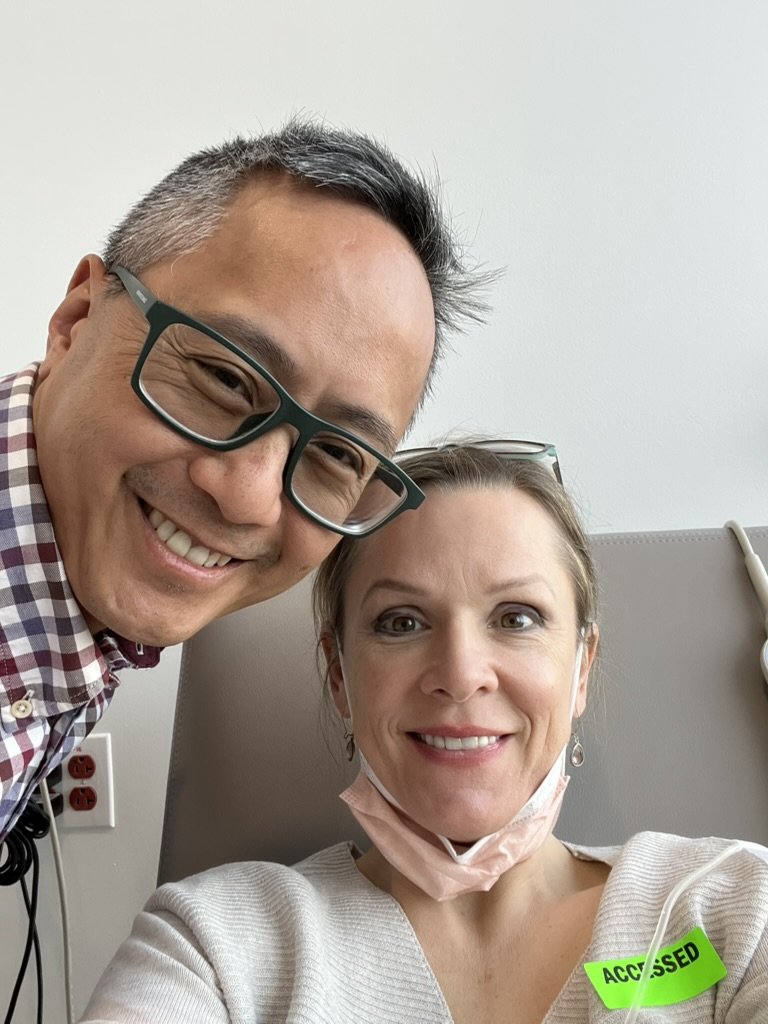
Before and after gadolinium toxicity: Photos taken 13 months apart (March 2023 and April 2024), following 4 MRIs with gadolinium.
The situation worsened as my eosinophil counts continued to climb, accompanied by elevated galectin-3 (a fibrotic biomarker), histamine levels, and tryptase levels (both allergy markers). Some of my red blood cells also began to show abnormalities, such as polychromasia and ovalocytes. I developed severe carpal tunnel syndrome due to tendon thickening, experienced significant muscle weakness, and lost subcutaneous fat. My red blood cell cholinesterase levels altered, my inflammatory marker D-dimer spiked, and my blood pressure rose dramatically. Each pulse projection felt like it was pounding in my brain. I also developed thoracic outlet syndrome. These are just a few of the many symptoms I experienced, all of which I documented meticulously for future research.
Despite seeking help from multiple healthcare providers, no one could explain
my elevated gadolinium levels in urine and hair analysis.
Steroid treatments provided only temporary relief (eosinophils would decrease) (see graph).
Cancer Diagnosis
Being diagnosed with stage 4 oncocytic kidney cancer in October 2022 profoundly changed the trajectory of my life. Cancer compelled me to deepen my faith, prioritize family, and focus on my health.
Initially, I tolerated the cancer medications and adapted well to the accompanying lifestyle changes. However, over time, troubling symptoms emerged that significantly impacted my quality of life. When I raised these concerns with my care team, they attributed everything to the cancer medications—Lenvatinib and Keytruda. While I remained “stable” for a time, subsequent MRIs with gadolinium coincided with a marked increase in my eosinophil levels (blood cells released during allergic responses).
In the acute phase, I was told by the doctors that the immunotherapy might have heightened my sensitivity to gadolinium, triggering mast cell activation. Sadly, I was never warned about these gadolinium-related risks before undergoing the additional MRIs.
I wouldn’t ever tell a fellow gadolinium-injured patient to do chelation or not to do chelation because it is a personal decision, but based on the severity of my case, I am not sure I would be alive without the treatment of gadolinium deposition disease.
Opportunities
I am profoundly grateful to God for being alive and for the opportunity to learn more through this journey. As a healthcare provider, I’ve realized the critical need for patients to access precision medicine, particularly when facing gadolinium-related issues. This past year was the hardest of my life—moments like struggling to remove my shoes, because my muscles were too weak were truly frightening. Not being able to tolerate downward postures, such as pulling weeds or tying my shoes or grooming the dog lead to blood pulling in my head and arms. Yet, through extensive research, I was able to piece together what happened.
Now, I am determined to help others understand this condition and these reactions. This is an opportunity to contribute to the growing body of scientific knowledge—because better knowledge leads to better outcomes.
We have a responsibility to our fellow human beings to fully understand the “medications” and treatments we use, including long-term and cumulative effects.
Watch Bridget’s Story.
Gadolinium toxicity is like an alternate universe. I have foreign magnetically-charged metal lanthanide in my body that is confusing my body. Gadolinium and calcium are about the same size in radius, but one is +3 charge and the other is +2 charge, which threw a monkey wrench into my body’s machinery. Further, gadolinium’s charge is +3 and phosphorus’s charge is -3. Our bodies operate on electrical charge impulses. All the normal structure and function biochemistry is thrown off. My body’s innate way of taking care of itself is thrown off. My Creator didn’t intend to have gadolinium coursing through my blood and lymphatic vessels. It isn’t in the design plan. I nearly died. Immune dysfunction related to gadolinium toxicity is poorly understood.
Prayer was my only hope.
-Bridget
Kidney Cancer Biomarkers
Unlike prostate cancer, where prostate-specific antigen (PSA) biomarkers alert physicians and patients to the presence of potential prostate cancer inflammation, kidney cancer lacks an FDA-approved biomarker for diagnosis and treatment monitoring. PSA was one of the first biomarkers used for cancer detection and continues to play a crucial role in assessing treatment effectiveness in prostate cancer patients. However, for kidney cancer, no equivalent laboratory test exists, making it more challenging to track the disease's status without invasive procedures.
As a result, kidney cancer patient care heavily relies on frequent radiological monitoring, including MRI and CT scans. While MRI gadolinium is excreted through the kidneys, which can be concerning for kidney function over time, CT scans expose patients to significant radiation and oxidative stress. Even with a good glomerular filtration rate, I found this monitoring paradigm difficult, as the risks associated with radiation exposure and contrast agents weigh heavily on patients already dealing with a complex and often aggressive disease.
However, there is hope for the future. Advances in technology may soon allow for the integration of imaging techniques with emerging biomarkers, enabling quicker and more accurate assessments of treatment effectiveness. Improved laboratory tests for kidney cancer could significantly transform patient care, offering a safer and more efficient approach to monitoring. If a kidney cancer biomarker were developed and approved, primary care physicians could easily order tests for patients at risk of relapse, providing a less invasive and more accessible way to manage the disease and its treatment. This evolution in healthcare could alleviate the burden of frequent radiological monitoring, reduce risks, and ultimately lead to better outcomes for patients.
Bridget’s Take on Gadolinium Toxicity:
Gadolinium toxicity may be rare, but it is dangerous, as it affects mitochondria, and can be stored in the liver, bone and brain, and can cause severe immunological symptoms. There is a FDA black box warning for gadolinium for good reasons. The CDC also warns about gadolinium. However, patients are routinely not made aware of the extent of the risks involved.
Cancer patients and oncologists make decisions based on how patients feel. Is there overlap of gadolinium-related symptoms and side effects of oncology medications? I had stopped immunotherapy because of the symptoms that were later clearly attributed to gadolinium. Are other patients having symptoms that are related to gadolinium rather than tyrosine kinase inhibitors and immunotherapy? This is an area that is in dire need of more research and understanding.
— Bridget