What is Gadolinium,
and why is it still in my body?
Image from: MP Materials, rare earth mining company
What is gadolinium?
Gadolinium is an rare earth heavy metal element that is mined from the earth’s crust. It originates from mines in China (largest producer), United States, and a few other countries.
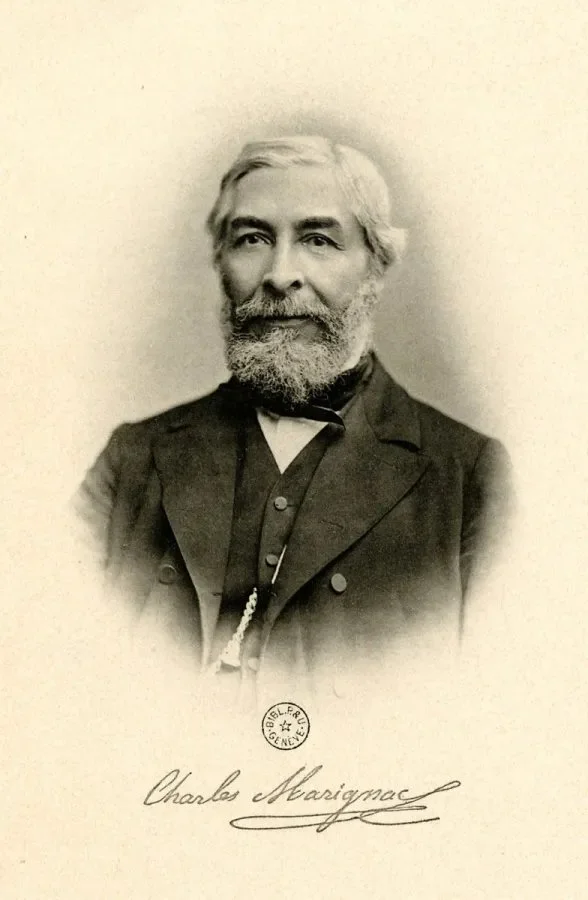
First identified in 1880 by Swiss chemist Jean Charles Galissard de Marignac, gadolinium is a silvery-white metal with unique magnetic and luminescent properties. Positioned at number 64 on the periodic table, it also has a strong affinity for water molecules.
How would a person acquire gadolinium toxicity?
Gadolinium is toxic to mammals, partly due to its magnetic properties. It has no biological function. Unlike essential minerals or common pathogens like viruses and bacteria, which the body has evolved to manage, gadolinium is an entirely foreign element with no reference history in human biology. As a result, while the body effectively eliminates excess metals to maintain fluid and electrolyte balance, gadolinium is instead retained in bones, organs, and soft tissues due to its unique chemical properties. Gadolinium also competes against calcium in biological functions, including enzymes, peptides, and metabolism. It can be devastating for those affected.
Gadolinium toxicity refers to the sometimes fatal condition that can occur when gadolinium deposits in the body after an MRI scan with a gadolinium-based contrast agent (GBCA).
Symptoms can vary but often include pain, brain fog, fatigue, and changes in skin or tissues. Not everyone who receives a gadolinium-based MRI experiences immediate toxicity, but in all individuals, gadolinium retains in the body and can potentially lead to adverse effects down the line.

Industrial Applications
Gadolinium serves no biological purpose, but it has benefits in industrial applications. It has been used in various industries, including:
Nuclear reactors: Due to its ability to absorb neutrons, gadolinium is used as a shielding material in nuclear reactors to help control nuclear reactions.
Electronics and phosphors: Gadolinium is used in phosphors that create the glow in color television screens and LED lights. It is also used in CDs and refrigerators.
Manufacturing alloys: When mixed with other metals, gadolinium can improve heat resistance, which is especially useful in jet engines and high-temperature applications. However, unfortunately, many toxicity sufferers have noted drops in their overall core temperature, indicating that its chemical properties have physiological detriments, too.
Gadolinium is responsible for thousands of cases of disability and death around the globe. FAERS reports around ~33,000 adverse events, a figure that contradicts a 2016 FOIA request. The true toll remains unknown.
The Introduction of Gadolinium in Medicine
Use in MRI Scans
In the 1980s, scientists discovered that gadolinium-based compounds could enhance MRI (Magnetic Resonance Imaging) scans. When bound to certain chemical agents (chelates), gadolinium’s magnetic properties allow it to provide greater contrast in MRI images, making it easier to view and diagnose issues in soft tissues, organs, and blood vessels.
Why gadolinium?
Gadolinium’s paramagnetic nature is utilized in MRI because it enhances the relaxation time of nearby water molecules in the body, thereby creating clearer images. Due to the chances for fatality when administering free gadolinium, gadolinium-based contrast agents (GBCAs) are attached to a ligand chelate that surrounds gadolinium in the hopes that gadolinium is expelled via the kidneys before detaching from this chemical cage. Unfortunately, this is not the case.
Growing Awareness of Gadolinium Retention
Concerns in the 2000s and 2010s
While gadolinium-based agents were initially advertised as safe, studies and patient reports in the 2000s and 2010s raised concerns about gadolinium retention in the body. Researchers, including Dr. Shawn Cowper, found that gadolinium could remain in the bones, brain, and other tissues long after it was administered. Although it retains for life in anyone who receives it, it can be especially fatal in people with compromised kidney function due to fibrosis of the skin and organs. This is called Nephrogenic Systemic Fibrosis, or NSF. In the decade and a half since these warnings came out, there have been numerous cases of fibrosis in individuals with normal renal function. Unfortunately, regulatory agencies have ignored the pleas from patients to be recognized, so the wider health community is wrongly informed that fibrosis is only possible in individuals with renal failure. The recognition of NSF, however, led to increased scrutiny of gadolinium-based agents.
Regulatory Responses
In 2017, after patients pushed for the FDA to acknowledge gadolinium deposition disease—referred to as “gadolinium retention” but dismissed as having no associated symptoms—the European Medicines Agency (EMA) took decisive action. The EMA outright banned linear gadolinium-based contrast agents due to safety concerns over gadolinium retention.
The FDA, on the other hand, issued a vague warning in 2017 about the risks of gadolinium retention, but unfortunately, these warnings were only made it to doctors and not to patients. By 2018, the FDA partially revoked its earlier warning, further diluting the message and failing to implement significant regulatory changes. To this day, the majority of people injured by gadolinium contrast never had informed consent.
Why does Gadolinium Stay in the Body?
Gadolinium is not found freely in nature. It has a very high affinity to bind with other metals. Our bodies are made up of essential minerals like: magnesium, zinc, and calcium.
Because gadolinium is very reactive, it can both displace these essential minerals in biological functions, and it can be attracted to natural chelators that are in our bodies, such as oxalates. Breaking out of the manufactured cage, the gadolinium molecules roam the body, wreaking havoc on the immune system in particular people. It interferes with enzymes and peptides.
RECENT YEARS
RECENT YEARS
Recent Years
The push for regulatory change included a 2017 FDA hearing where individuals courageously shared their life-altering experiences with gadolinium toxicity. While label changes for gadolinium-based contrast agents were implemented following the hearing, the FDA does not enforce these recommendations. This lack of enforcement has allowed facilities to continue misleading patients about the safety of gadolinium contrast dye, contributing to a growing number of cases of harm and disability from its toxic effects.
In 2020, as a follow up to the FDA hearing, Sharon Williams from GadoliniumToxicity.com wrote an open letter to the Food and Drug Administration that describes gadolinium toxicity, including burning pain, numbness, tingling, electric-like sensations, muscle twitches, weakness, dry eyes, gastrointestinal issues, extreme fatigue, cognitive dysfunction ("brain fog"), tinnitus, and skin changes, and more. She links multiple diseases and systemic organ involvement to gadolinium toxicity. As of 01/10/2025, Sharon has still not heard back from the FDA.